- About
- Return to Menu
- Our Ingredients
- Our Approach
- The Science Behind The Diets
- Learn
- Shop
- Webinars
- Return to Menu
- Bladder Health in Cats
- Obesity, Diabetes, & Metabolic Disorders in Cats
- Chronic Kidney Disease in Cats
- Digestive Health in Canines
- Diet’s Foundational Role in Supporting a Dog with Cancer
- Diets Foundational Role In Supporting Your Dogs Skin Health
- Diet’s Crucial Role in Caring for the CKD Dog
- Contact
- For Veterinarians
- Reset Password
- Login

- Cart
- Return to Menu
- Return to Menu
- Return to Menu
- Return to Menu
Kidney Disease in Cats
A Chronic Kidney Disease (CKD) diagnosis can be accompanied by many unknowns for guardians and can lead to a lot of questions, confusion, and concern. Though CKD is one of the most common medical conditions in cats– approximately 3 out of 10 cats develop chronic kidney disease in their lifetime– with the right treatment protocols and care, cats can often live full lives after a CKD diagnosis.
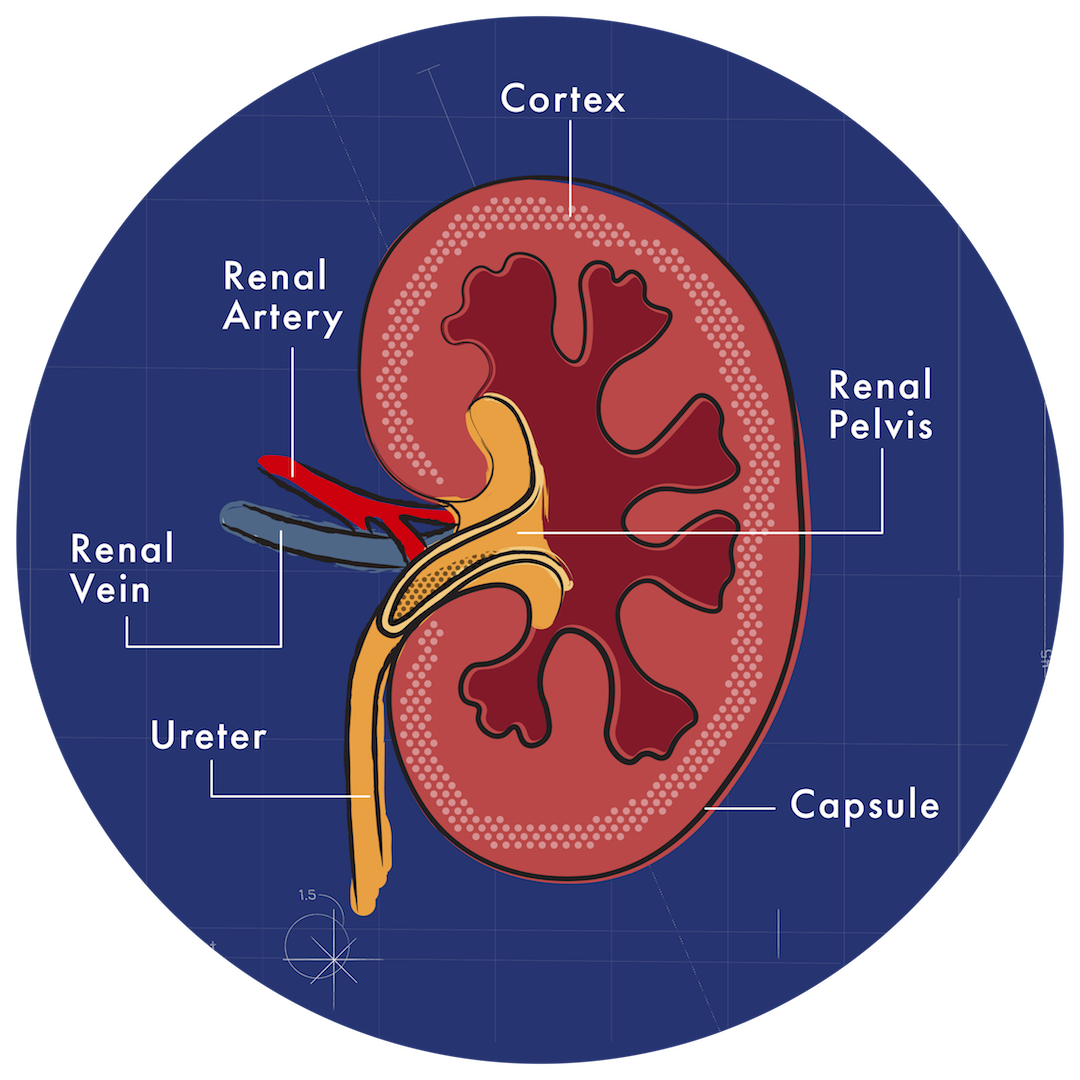
The Role The Kidneys Plays
The kidneys are filtration systems. These two bean-shaped vital organs are tasked with conserving crucial minerals, disposing of harmful byproducts, controlling water balance and body fluids, pH levels, and blood pressure, and producing hormones like erythropoietin.
Kidneys also function to ensure calcium to phosphorus balance.
What is Kidney Disease?
Kidney (renal) disease is a broad term for any disease process that leaves the kidney unable to filter toxins out of the body and maintain water balance in the body.
When the kidneys do stop functioning properly, waste byproducts build up in the body, causing more health problems, making your cat feel sick, and in later stages of disease progression, renal failure.
Types of Kidney Disease
Acute Renal Failure
Kidney function suddenly declines within a week or months. Generally, infection or ingesting a toxin like antifreeze, pesticides, or cleaning products causes acute renal failure. Even too much vitamin D can be poisonous to your cat’s organs.
Chronic Renal Failure
The loss of function is a slow progression, happening gradually over years.
What are the Stages of Chronic Kidney Disease in Cats?
CKD is often referred to as early, moderate, or advanced, though it’s also numbered 1-4, 4 being the most severe. The International Renal Interest Society (IRIS) staging system created these stages to judge the severity of the kidney disease. The higher the stage number, the more signs you’ll see in your cat.
Stages are set by the creatinine levels, so when creatinine is at X, your cat is in stage 1; when it’s Y, the cat is in stage 2.
Ultimately, being proactive and getting annual bloodwork can identify subtle changes in the body long before they start showing symptoms of kidney dysfunction.
In the beginning stages of renal disease, the concern is dehydration because kidneys are not conserving fluids and producing dilute urine. The kidneys cope with their inability to filter toxins and byproducts by producing a larger amount of more dilute urine. You may notice your cat drinking more and spending more time in the litter box.
Disease progression causes a cascading effect in the body, dominoes falling one after another. Toxins built up in the body will increase, and the symptoms will worsen, damaging kidney function and progressing the severity of the disease.
When the kidneys aren’t working well, all systems in the body are also affected – the heart, liver, and pancreas, even blood pressure. High blood pressure (hypertension) occurs in as many as ⅔ of all CKD cases. However, this may be an instance of the chicken or the egg since hypertension worsens kidney function, and a progressive decline in that function can lead to poor blood pressure control.
What’s important to remember is that a diagnosis shouldn’t send you spiraling. Focusing on the stages, the numbers, or lab results can be overwhelming. Instead, focus on what you can do for your cat’s quality of life.
What are the Signs of Chronic Kidney Disease in Cats?
The initial signs can include:
- Drinking and urinating more and spending more time in the litter box
- Weight loss/loss of appetite
- Lethargy
- Vomiting
- Diarrhea
- Decreased self-grooming
- Poor coat quality
Signs of advancing kidney disease include:
- Dehydration – severe dehydration
- Increased water consumption and urination
- Lethargy progressing in severity
- High blood pressure
- Increased loss of appetite, anorexia, or weight loss
- Diarrhea
- Blood in the urine
- Neurological signs, including seizures due to high ammonia levels in the blood
Most guardians don’t notice CKD symptoms until 70+ % of function is lost because the kidneys have ample capacity to perform their various functions. That means at least two-thirds of the kidneys must be dysfunctional before you see any signs.
What Causes Chronic Kidney Disease in Cats?
Often the cause is unknown or difficult to pinpoint because the onset is slower, and many different conditions can cause it. Your cat’s body is interconnected, so when one system has problems, it can often lead to issues elsewhere.
The potential CKD causes are:
- Urine blockages
- Chronic Dehydration
- Dental disease
- Genetic predispositions
- Acute chronic failure from kidney poisoning
- Autoimmune diseases
- Diabetes
- Severe dehydration
- Toxins
How is CKD Diagnosed?
Signs like weight loss, weakness, and poor coat quality can be seen with many other diseases, so blood and urine tests are needed for a diagnosis. The blood tests will look for elevations in creatinine and Blood Urea Nitrogen (BUN), which are indications of the kidney not filtering out these waste chemicals. Mild elevations of creatinine and BUN can be from dehydration, but repeated or high levels are diagnostic for kidney disease.
New blood tests like SDMA– a genetic marker of kidney function- can help identify kidney disease early, sometimes years before signs show. Many veterinarians include it in annual wellness screenings, so you could ask at your next appointment.
There’s no cure for CKD, and the disease is progressive, but the earlier CKD is diagnosed, the more time you have to be proactive about his care and potentially delay the disease’s progression with proper nutrition. Consider annual bloodwork checking BUN, creatinine, phosphorus, and potassium for cats greater than 8 years old to develop a baseline and for early detection.
Diet’s Role in CKD Care
Fluid therapy and diet are the staples in treating chronic kidney disease. Cats can live for years when the disease is caught early and a care plan is put in place.
A CKD diet aims to nourish the body and protect the kidneys by lessening their workload.
The currently accepted approach to this is Low Protein / Low Phosphorous diets.
The low protein approach started because of a general thought that urea, the waste product of protein, was taking a toll on the marginal kidney. And that reducing the amount of dietary protein would reduce the levels of urea. Urea is excreted by the kidney and marginal kidney function can lead to a buildup of urea in the blood. One of the indicators of kidney health is the levels of urea in the blood called blood urea nitrogen or BUN.
But no studies have shown that restricting protein will prevent further deterioration of kidney function in dogs and cats—quite the opposite. On restricted protein diets CKD patients were not able to meet their protein needs. Inadequate amino acids can lead to muscle breakdown. This breakdown of muscle will cause an increase in creatinine which the kidneys have to clear, along with muscle-wasting, which can be mistaken for worsening CKD in these patients.
The current school of thought is that moderate amounts of high-quality, animal-based proteins are needed to nourish the body while not overtaxing the kidney function.
Dr. Pierson agrees. “With regard to how protein affects the kidneys, it’s important to understand protein is not the enemy of the cat kidney. Protein doesn’t cause kidney disease. It doesn’t exacerbate kidney disease. It is not the enemy of the kidney.”
Dr. Judy Morgan also agrees with this sentiment, “Many veterinarians will immediately recommend a protein-restricted diet in pets with any stage of kidney disease. Protein should not be restricted in early stages of kidney disease, as this will result in muscle wasting and weakness.”
As does Dr. Karen Becker, “Many veterinarians still insist that a renal diet should be low in protein, despite studies showing aging pets — including those with kidney disease — need more protein, not less. But it has to be very high-quality protein.”
As carnivores, cats and dogs need lots of high-quality protein to maintain organ and immune function and healthy muscle mass.
All ingredients in your cat’s food should be fresh, highly bioavailable, easily digested, and highly palatable.
The Importance of Real Whole Food Nutrition in a Chronic Kidney Disease Diet
In the feline kidney patient, the goal is to minimize phosphorus levels while nourishing the carnivore’s body with moderate amounts of high-quality animal protein. We also want to support kidney function with proper ratios of Omega-3 fatty acids and replenish losses from the symptoms of CKD. All can be accomplished with clean whole food nutrition.
The quality and source of protein are very important to a feline suffering from CKD. Moderate amounts of clean, wholesome meats and organs are easily absorbed providing the CKD patient with the necessary amino acids to prevent weight loss or cachexia. This approach will nourish the body and support the best quality of life. Meats also contain a lot of fluid in a form that the carnivore cat is designed to utilize.
In the case of kidney patients, something as simple as an egg can provide precisely what the body needs. Ingredients like eggs are multi-functional. The egg itself is a complete protein and low in phosphorus, and the shell is rich in calcium carbonate, which binds phosphorus to the gut so it can be eliminated. Doing so lightens the kidney’s workload and reduces the ill effects of the compromised organ.
The correct blend of skeletal meats (chicken), organs (liver and gizzards), and rice can lead to the reduced levels of phosphorus. This delicate balance can nourish the carnivore without taxing the kidney.
Controlled phosphorus protects kidney function and can be accomplished in two ways. One way to control phosphorus is through reduced phosphorus content in the food. The second way is through binding the phosphorus in the gut. The first approach can be attained through correct proportions of nourishing whole foods, which in proper combinations have reduced levels of phosphorus. The second approach is accomplished by selecting the correct foods to bind phosphorus, such as chitosan and calcium carbonate, via cooked ground eggshells.
Omega-3 fatty acids help decrease inflammation throughout the body. All cats can benefit from them, but especially cats with chronic diseases caused by inflammation such as CKD.
Ideally, these omega-3 fatty acids will come from marine sources. Omega-3 fatty acids are some of nature’s strongest anti-inflammatories and are paramount for cats. In addition to being anti-inflammatory, Omega-3 fatty acids are crucial for immune, nervous system, and kidney functions.
Ground krill is a rich source of these omega-3 fatty acids. And unlike fish oils, krill is so low in the food chain that they do not accumulate toxins that can be found in larger fish.
CKD patients have an increased voiding of dilute urine. This water loss can accompany a loss of water-soluble B vitamins and potassium. Potassium and B vitamins must be added to replace those losses.
Water helps with digestion, circulation, and other bodily processes like perfusion (movement of fluids through the organ), which helps move the harmful byproducts through the filtration system and out of the body.
The right nutritional framework not only nourishes the body but can slow the progression of the disease, and that can drastically impact the lives of cats with CKD for the better.
Note: The information provided is educational and does not represent medical advice regarding pets. Please see your vet for an accurate diagnosis of your pet’s condition.
- Automatically re-order your favorite products on your schedule.
- Easily change the products or shipping date for your upcoming Scheduled Orders.
- Pause or cancel any time.

